Abstract
Background
Improved quality of life and overall satisfaction of care stems from patients’ understanding of their disease state and collaboration with their providers in shared decision-making (SDM). Using a validated collaborative learning model (Sapir 2017), we evaluated patient and healthcare provider (HCP) perceptions regarding SDM and chronic lymphocytic leukemia (CLL) care.
Methods
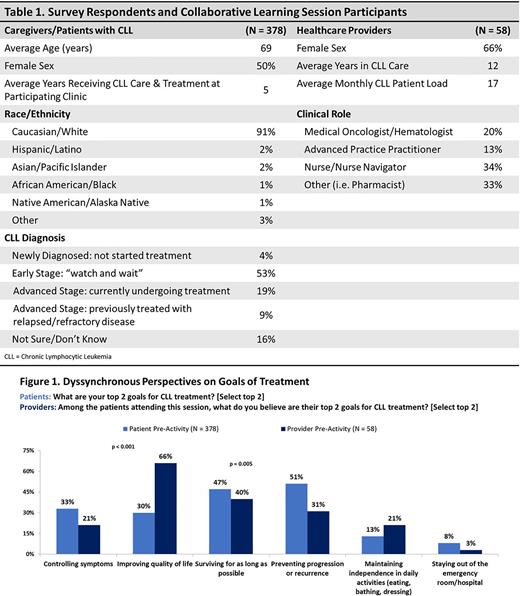
From October to November 2020 and September to November 2021, we conducted two collaborative patient-provider programs involving 12 oncology centers across the US. A combined 378 patients and caregivers of patients with CLL and 58 HCPs participated in the programs (Table 1). Before and after the sessions, patients and their providers completed tethered surveys to assess alignments and discordances in preferences, experiences, and concerns around CLL treatment and SDM. Chi-square analysis was used to test significance between patient and provider responses.
Results
Patients and HCPs were aligned in the factors they thought were most important to patients in treatment decision-making, identifying how well the treatment will work against my cancer (58% patient, 50% HCP) and how it will affect my quality of life (42% patient, 43% HCP) as most important. However, HCPs’ perceptions of the biggest challenges faced by patients with CLL in their care differ from patient self-reports. HCPs believe their patients’ biggest challenge in CLL care is worrying about and/or difficulty managing side effects from treatment (40%) whereas, patients most often reported their biggest challenge as "other” (50%).
When asked about their patients’ top goals of treatment, HCPs compared to patients placed higher importance on improving quality of life (66% vs 30%, p<0.001) and maintaining independence in daily activities (21% vs 13%). Conversely, HCPs were less likely than patients to identify patients’ goals of treatment as preventing disease progression (31% vs 51%, p = 0.005), surviving for as long as possible (40% vs 47%), and controlling symptoms (21% vs 33%) (Figure 1).
Patients and HCPs also differed in their estimates of how involved they feel in decisions around treatment options. HCPs reported only 39% of their patients’ being very or extremely involved in their care compared to 67% of patients. When asked why patients are not more involved in treatment decisions, patients were more likely than HCPs to report that they are already fully involved in treatment decision-making (45% vs 12%).Conversely, HCPs were much more likely to report that patients feel too overwhelmed to make decisions (57% vs 3%) and that patients lack of understanding of medicine (36% vs 5%). In addition, 8% of patients acknowledged less involvement because their care team does not ask about their treatment goals and priorities. Providers cite top barriers to engaging patients with CLL in SDM as not enough time (62%) and patients’ low health literacy (34%).
HCPs were more likely than patients to report that they always/often: askhow CLL is affecting the patient's quality of life (64% vs 54%) and ask about the patient's goals for treatment (52% vs 43%). Patients reported higher rates of providers willing to work with the patient to create a treatment plan that fits the patient's needs and goals (59% patients, 52% HCPs). When asked about their experience with clinical trials, 78% of patients stated no experience.
Following the collaborative learning sessions, patients set goals to notify their care team if new symptoms arise or if I have concerns (55%), consider their treatment options more closely (41%), and discuss goals for treatment with the care team (35%). HCPs made commitments to engage their patients more frequently in SDM (83%), increase the variety of educational materials they provide to patients (50%), and conduct additional small-group education sessions with their patients (50%).
Conclusions
Patients with CLL and their HCPs differed in their experiences, perceptions, and beliefs related to SDM and other key aspects of patient-centered care. Collaborative education can support improved knowledge, communication, and understanding between patients and providers, leading to greater engagement in SDM around personalized CLL care.
Study Sponsor Statement
The study reported in this abstract was funded by an independent educational grant from Genentech. The grantor had no role in the study design, execution, analysis, or reporting.
Disclosures
Davids:Ascentage Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Adaptive Biotechnologies: Consultancy, Membership on an entity's Board of Directors or advisory committees; Bristol-Myers Squibb: Consultancy, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Merck: Consultancy; Ono Pharmaceuticals: Consultancy; Research to Practice: Honoraria; Eli Lilly and Company: Consultancy, Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; AbbVie: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Research Funding; BeiGene: Consultancy, Membership on an entity's Board of Directors or advisory committees; Verastem: Consultancy, Research Funding; TG Therapeutics: Consultancy, Research Funding; Takeda: Consultancy; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal